LSD’s grip on brain protein could explain drug’s long-lasting effects
Locked inside a human brain protein, the hallucinogenic drug LSD takes an extra-long trip.
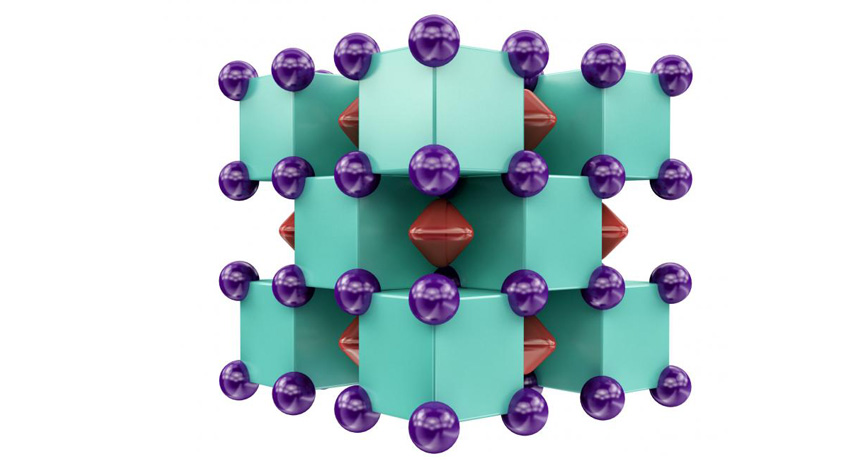
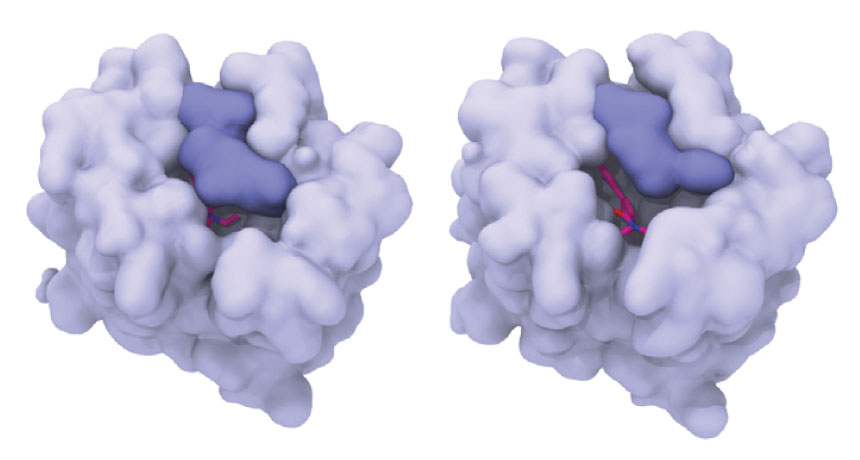
New X-ray crystallography images reveal how an LSD molecule gets trapped within a protein that senses serotonin, a key chemical messenger in the brain. The protein, called a serotonin receptor, belongs to a family of proteins involved in everything from perception to mood.
The work is the first to decipher the structure of such a receptor bound to LSD, which gets snared in the protein for hours. That could explain why “acid trips” last so long, study coauthor Bryan Roth and colleagues report January 26 in Cell. It’s “the first snapshot of LSD in action,” he says. “Until now, we had no idea how it worked at the molecular level.”
But the results might not be that relevant to people, warns Cornell University biophysicist Harel Weinstein.
Roth’s group didn’t capture the main target of LSD, a serotonin receptor called 5-HT2A, instead imaging the related receptor 5-HT2B. That receptor is “important in rodents, but not that important in humans,” Weinstein says.
Roth’s team has devoted decades to working on 5-HT2A, but the receptor has “thus far been impossible to crystallize,” he says. Predictions of 5-HT2A’s structure, though, are very similar to that of 5-HT2B, he says.
LSD, or lysergic acid diethylamide, was first cooked up in a chemist’s lab in 1938. It was popular (and legal) for recreational use in the early 1960s, but the United States later banned the drug (also known as blotter, boomer, Purple Haze and electric Kool-Aid).
It’s known for altering perception and mood — and for its unusually long-lasting effects. An acid trip can run some 15 hours, and at high doses, effects can linger for days. “It’s an extraordinarily potent drug,” says Roth, a psychiatrist and pharmacologist at the University of North Carolina School of Medicine in Chapel Hill.
Scientists have known for decades that LSD targeted serotonin receptors in the brain. These proteins, which are also found in the intestine and elsewhere in the body, lodge within the outer membranes of nerve cells and relay chemical signals to the cells’ interiors. But no one knew exactly how LSD fit into the receptor, or why the drug was so powerful.
Roth and colleagues’ work shows the drug hunkered deep inside a pocket of the receptor, grabbing onto an amino acid that acts like a handle to pull down a lid. It’s like a person holding the door of a storm cellar closed during a tornado, Roth says.
When the team did additional molecular experiments, tweaking the lid’s handle so that LSD could no longer hang on, the drug slipped out of the pocket faster than when the handle was intact. That was true whether the team used receptor 5-HT2B or 5-HT2A, Roth says. (Though the researchers couldn’t crystallize 5-HT2A, they were able to grow the protein inside cells in the lab for use in their other experiments.) The results suggest that LSD’s grip on the receptor is what keeps it trapped inside. “That explains to a great extent why LSD is so potent and why it’s so long-lasting,” Roth says.
David Nutt, a neuropsychopharmacologist at Imperial College London, agrees. He calls the work an “elegant use of molecular science.”
Weinstein remains skeptical. The 5-HT2A receptor is the interesting one, he maintains. A structure of that protein “has been needed for a very long time.” That’s what would really help explain the hallucinogenic effects of LSD, he says.